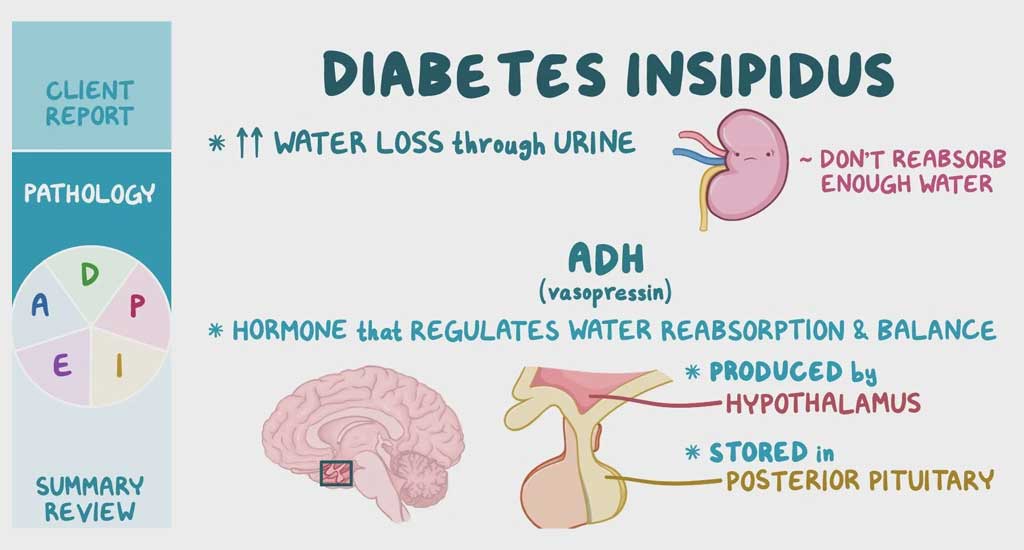
Diabetes insipidus is a derivative of the Latin word In + Sapid, meaning not tasty/tasteless. A major symptom of this uncommon condition is excessive urination, which is pale and diluted. This condition is different from diabetes mellitus, in which patients have consistently high glucose levels in their blood. In diabetes insipidus, a patient’s blood sugar levels are normal, but their kidneys cannot concentrate urine properly.
What is Diabetes Insipidus?
Diabetes insipidus can be described as a condition caused due to an electrolyte imbalance in the body. One of its characteristic features is the inability of the kidneys to function properly, causing excessive urination and reducing the re-uptake of fluids from the kidneys. In this condition, your kidneys are unable to conserve water.
However, this condition should not be confused with diabetes mellitus 1 or 2 as the latter causes increased blood sugar levels. In contrast, diabetes insipidus leads to an imbalance between salt and water in the body. So if you are wondering what causes low blood sugar or high blood sugar, the answer is definitely not diabetes insipidus.
Diabetes Insipidus Causes
Our kidneys filter the body fluids several times a day. Usually, most of the water is absorbed by the body, and a small amount is excreted as concentrated urine. In diabetes insipidus, the kidneys cannot re-uptake the water back into the body system, ultimately causing loss of large amounts of water from the body and causing an electrolyte imbalance. Diabetes insipidus can be of four types. The causes of diabetes insipidus vary as per the type, listed below:
i) Central Diabetes Insipidus: This type of diabetes insipidus occurs when the body has a lower than average amount of antidiuretic hormone called vasopressin. The water amount excreted by the kidneys is controlled by vasopressin. Vasopressin is synthesised in the hypothalamus of the brain. It is stored and released by the pituitary gland in the brain’s basal part. Central diabetes insipidus is primarily seen to start in the 10-20 age group.
The various causes that lead to central diabetes insipidus are:
- Genetic disorder
- Head injuries
- Brain infections
- Brain surgeries that cause collateral damage to the pituitary gland
- Blood supply issues
- Tumour growths near or on the pituitary gland
- Autoimmune diseases that damage vasopressin secreting cells
ii) Nephrogenic Diabetes Insipidus: This type is caused by the reduced or failed response of the kidneys to the release of vasopressin. This usually happens due to kidney defects.
Nephrogenic diabetes insipidus can result from:
- Certain medications
- Chronic kidney disease
- Low potassium levels in the blood
- Hypercalcemia (excess calcium in the body)
- Kidney diseases like polycystic kidney disease
iii) Dipsogenic Diabetes Insipidus: This condition is caused due to excessive intake of fluids due to the faulty hypothalamic thirst response. It happens when the hypothalamus repeatedly signals the body for thirst due to some damage to it. Dipsogenic diabetes insipidus can be caused due to
- Mental illnesses
- Use of desmopressin
iv) Gestational Diabetes Insipidus: This type of diabetes insipidus happens during pregnancy and usually resolves postnatally. Pregnant women make vasopressinase in the placenta, which can break down vasopressin. Therefore, it has a higher chance of occurrence in pregnancy-related ailments like pre-eclampsia or pregnancy-related fatty liver. If a pregnant woman is diagnosed with diabetes insipidus, she should be given prompt treatment, as it may be fatal for the mother and the baby. So what causes gestational diabetes insipidus?
- In cases where the disease runs in the family
- The way your body controls thirst
Diabetes Insipidus Symptoms
The following are the symptoms of the rare condition:
- Increased thirst: Due to the loss of large amounts of water, the patient experiences increased hunger and fatigue due to dehydration. The patient also has an uncontrolled desire for cold or ice water.
- Excess urination: The patient can experience high volumes of very pale and diluted urine. This can happen almost every hour of the day. Excess nocturnal urination also leads to disturbed sleep.
Diabetes Insipidus Complications
The possible complications of diabetes insipidus include:
- Severe dehydration
- Seizures
- Weight changes
- Vomiting
- Appetite loss
- Growth restrictions
- Long-term cases can cause hypokalemia
- Depression
Diabetes Insipidus Treatment
If you have symptoms of diabetes insipidus, your doctor may ask you to get some tests done to decide on treatment protocol and prognosis. Particular diabetes insipidus causes directly affect the type and mode of treatment.
Test requirements
- Osmolality and blood sodium
- Desmopressin challenge
- Head MRI
- Serum Co-protein levels
- Urine analysis
- Urine concentration
- Urine output
Treatment Options in Diabetes Insipidus
The treatment will depend on the type of diabetes insipidus you have:
- Vasopressin (injections, tablets, nasal spray) can help treat central Diabetes Insipidus.
- Nephrotic diabetes insipidus, caused due to a specific medication, may reverse itself if the medication is discontinued. However, medications taken for years can cause permanent nephrotic diabetes insipidus.
- Nephrogenic diabetes insipidus caused due to an infection may require anti-inflammatory medicines and diuretics (medications that regulate water balance in the body).
- Hereditary diabetes insipidus or lithium-induced diabetes insipidus may require treatment with medications that reduce urination. In addition, the patient would need to increase water intake to match the water loss.
Diabetes insipidus patients may need monitoring for continued loss of water even after treatment.
- To see if thirst levels are manageable.
- Vasopressin therapy patients will need monitoring of fluid intake and thirst control.
- Six monthly tests to check electrolyte balance.
Excessive water consumption may cause dilution of electrolytes, and this can be what causes low blood sugar in diabetes insipidus patients who do not have diabetes mellitus.
Conclusion
It is recommended to consult your primary health care provider if you have symptoms that point towards diabetes insipidus. There are treatments available for diabetes insipidus when diagnosed and followed up at the right time. It is generally not a life-threatening condition if appropriately monitored, and patients can live everyday life with the help of medicines and changes in dietary habits. In cases where the underlying causes for diabetes insipidus is treated promptly, it hardly leads to severe health problems.